Diabetes Management
Program at HCPSC
Good care starts with educating people. HCPSC offers a free diabetes prevention program in English and Spanish for community members at risk of developing Type 2 diabetes. It is simple to qualify for the program by completing a 1-minute survey or having a hemoglobin A1C result between 5.7% and 6.4%, which indicates prediabetes.
The course is based on the National Diabetes Prevention Program and emphasizes lifestyle modifications to help minimize the chances of developing Type 2 diabetes. The steps include learning simple, easy-to-follow tools that will assist the participant in increasing physical activity and reducing weight.
Studies have shown that adhering to this program can reduce the likelihood of developing Type 2 diabetes or the complications associated with diabetes by 58%.

HCPSC diabetes prevention program has gained Full Plus recognition from the CDC and is facilitated by some certified lifestyle coaches trained through the DTTAC National Diabetes Prevention training program.
You can take the survey to determine if you have prediabetes. If this result is positive, you qualify to enter the program free of cost.
HCPSC Diabetes Management Services
At HCPSC, you can get access to a range of specialty services for the management of Type 1 and Type 2 diabetes. These services range from managing cases of hypoglycemia and hyperglycemia in the emergency department to offering nutritional advice and emotional support to diabetic patients.
In addition to inpatient diabetes services, HCPSC also provides high-quality hospital care for diabetics that include treatment of health issues that may arise due to diabetes.
At the hospital, you will be thoroughly checked by medical professionals to rule out any complications you may have developed due to high blood sugar levels. You may also be referred to another specialty department if you have an underlying condition that needs proper management, such as high blood pressure, kidney disease, or diabetic retinopathy.
With experienced healthcare professionals and the latest medical technology, patients can be assured that they are receiving the best care possible at HCPSC.
Diabetes & COVID-19
Since the emergence of the pandemic, there have been growing concerns about the impact of the virus on people with diabetes.
Diabetes is a condition that weakens the immune system, making it more difficult for our body to fight COVID-19 if not controlled.
The complications may range from mild to severe difficulty in breathing to pneumonia and even organ failure.
Due to the potential complications from contracting COVID-19, people with diabetes must take extra precautions to minimize their risk of getting seriously ill.
One of the most crucial precautions to take is to ensure that one gets vaccinated against the coronavirus as soon as possible.

COVID-19 vaccines have been formulated not only to prevent severe symptoms but also to reduce the risk of transmission of the virus.
Many other factors can affect a person’s susceptibility to COVID-19, such as;
 Age
Age
 Underlying health conditions
Underlying health conditions
 Lifestyle factors
Lifestyle factors
Healthcare workers must work harder than ever to help people with diabetes manage their condition more proactively and take necessary steps to stay healthy during these uncertain times.

Diabetes Stats in the United States
Currently, 37.3 million people in the United States have diabetes, one out of every ten people.
Among this population, 8.5 million live with an undiagnosed case of diabetes [2]. This means they are not receiving any treatment to manage this condition!
Moreover, it is projected that by 2050, about one-third of all adults in the US will be affected by diabetes.
This figure is seriously concerning and highlights the need for increased awareness and prevention efforts, particularly during the COVID-19 pandemic.
According to the American Diabetes Association, about 95% of all cases with diabetes are Type 2.
The most common risk factor among this population is obesity.
This explains why your physician always insists on maintaining a healthy diet and being physically active.
What is even more alarming is that the number of people under age 20 with a known case of Type 2 diabetes has significantly increased in the past two decades.
It is estimated that if the trend continues, this number will increase by 675% by 2060!
Uncontrolled hyperglycemia for longer durations may cause complications like nerve damage, kidney disease, vision impairment, and even premature death.
The above stats are pretty alarming, and therefore, it is crucial for individuals with diabetes to;
- Maintain reasonable blood sugar control,
- Get tested for COVID-19 immediately if they are experiencing symptoms, and
- Communicate regularly with their healthcare provider for routine checkups
Are People With Diabetes More Likely to Contract the Virus?
There is insufficient data to infer that people with diabetes or prediabetes are more or less likely to be infected by the coronavirus. We now know that anyone can get COVID-19, but people with a compromised immune system are more likely to be infected.
And if you have diabetes, you are more likely to be affected by the complications caused by this virus, which may lead to severe health conditions.
We outlined those facts not to worry you but to enable you to manage your condition more proactively.
The good news is with more experience and knowledge about the virus, medical professionals are becoming better equipped to handle cases and provide more effective treatments!
Moreover, the overall mortality rate due to COVID-related complications is decreasing with time as more people become infected and survive the disease with proper and timely management.
Developing Type 2 Diabetes After COVID-19
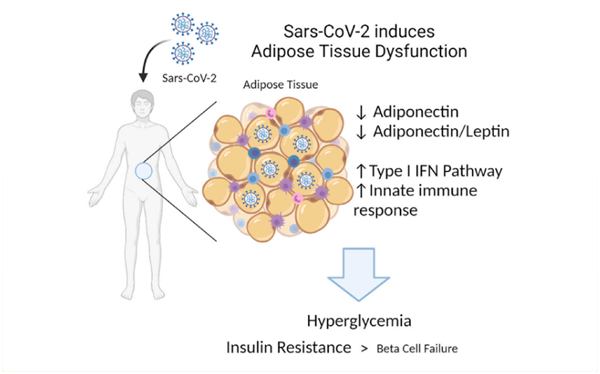
There is evidence to support that COVID-19 can bring out hyperglycemia in patients, particularly ones that have been hospitalized [5].
However, research is still needed to understand the potential implications of COVID-19-related hyperglycemia fully.
It is believed that acute inflammation and treatment with steroids are the two main culprits that may make an individual develop Type 2 diabetes [see figure above].
According to a study published in March 2022, people who have contracted the coronavirus have an increased risk of developing incident diabetes up to a year later. This is true regardless of how mild or severe their case of infection had been [1].
Earlier in November 2020, the results of a study were published in the journal Diabetes, Obesity, and Metabolism, according to which about 14.4% of individuals who developed COVID-related complications and had been hospitalized were later diagnosed with diabetes [3].
This data is sufficient to infer that there is a strong possibility of developing Type 2 diabetes mellitus after COVID-19.
You must also know that people already at risk of developing diabetes due to obesity, lack of physical exercise, and genetic reasons are susceptible to being diagnosed with Type 2 diabetes early after COVID-19.
Inflammation from cytokine activation is one of the primary causes of hyperglycemia in COVID-19 patients.
Cytokines are proteins that are released by immune cells in response to infection.
In COVID-19 patients, the immune system goes into overdrive, leading to an excessive release of stress hormones (endogenous steroids and catecholamines), which in turn causes hyperglycemia.
And when there are uncontrolled high blood sugar levels for a prolonged period, it eventually leads to Type 2 diabetes in these individuals.
The risk is even higher for patients who are obese and have a family history of diabetes mellitus.
It is, therefore, imperative to consult your physician if you have had COVID-19, have been diagnosed with prediabetes, or are taking medications to prevent an onset of diabetes.
Warning Signs You May Have Diabetes
It is important to note that contracting the coronavirus does not necessarily mean a person has also developed diabetes.
As we have already pointed out, some risk factors make an individual more vulnerable, such as obesity and a family history of Type 2 diabetes.
It is still a good idea to be watchful of diabetes symptoms even if you don’t fall in the high-risk category.
Some warning signs that indicate that you have diabetes include:
- Frequent urination, especially at night
- Excessive thirst
- Loss of appetite
- Sudden weight loss
- Weakness and fatigue
- Blurry vision
- Skin problems, mainly dehydrated skin
- A feeling of numbness in hands and feet
Watch out for these signs and symptoms and immediately get in touch with your healthcare provider if you experience them, especially after having had COVID-19.
Prevention of Diabetes
After COVID-19
There are some precautionary measures you MUST adhere to after contracting the coronavirus, especially if you:
- Have a family history of diabetes
- Are obese
- Have an abnormal BMI Suffer from metabolic disorders or other comorbid diseases, such as
- hypertension, sleep disorders, and abnormal lipid profile
Preventive measures, such as maintaining a healthy diet, exercising regularly, and monitoring blood sugar levels, can ensure a slow progression to Type 2 diabetes if you have prediabetes.
Here are a few things you can do to prevent diabetes after COVID-19:
Lose weight
If you are overweight, it is recommended that you lose 5-7% of your body weight after you recover from COVID-19 to minimize your risk of developing diabetes.


Follow a regular workout plan
You should start doing that now if you still need to follow an active lifestyle. Make a goal of obtaining 150 minutes of activity per week.
Adjust your pre-COVID diet
Evaluate your pre-COVID diet, and cut down on everything that causes unhealthy weight gain, such as sugars and carbohydrates.


See a physician
Consult your physician and get tested for diabetes right after you recover from COVID-19. Get tested again after 3 to 6 months and then once every year.
Sometimes doctors advise anti-diabetic medicine as prophylactic management of prediabetes in people with a strong positive family history of the disease and obesity. However, the most effective management of prediabetes is a lifestyle change program, such as the National Diabetes Prevention Program offered at HCPSC.
These preventive steps can make your progression to Type 2 diabetes considerably slow even if you get COVID-19.
Getting your vaccinations and boosters on time is also recommended so there is minimal risk of contracting the virus again.
What Happens If Someone With Diabetes Gets COVID-19?
While timely diagnosis and proper management ensure a smooth recovery from COVID-19 in most cases, the situation is a bit more alarming if you have diabetes.
You need to know that people with diabetes may experience severe COVID-19 symptoms and may also develop serious health conditions even after recovering from the infection.
Especially if you’re not vaccinated against the virus, you may develop these complications.
Some of these include; [4]
- Pneumonia,
- Acute respiratory failure
- Acute liver/cardiac injury
- Bacterial infections,
- Septic shock.
These complications can also be life-threatening, particularly if someone has another underlying health condition, such as heart disease.
In addition to the above-mentioned complications, diabetic ketoacidosis, or DKA, is a serious condition that all diabetic patients must be aware of.
This condition is more common in Type 1 diabetes. DKA is also closely related to sepsis and septic shock because the former makes it challenging to manage fluid intake and electrolyte levels in the body.
You need to be aware of the signs and symptoms of DKA and must also get your lab tests done to measure the level of ketones in your blood. If the number is moderately high, you must seek medical help immediately.
If you manage your diabetes well, the risk of developing the above-mentioned complications is significantly low.
How to Recover From COVID-19 If You Have Diabetes?
First of all, seek medical help immediately if you have contracted the virus and you also take other medications like:
- insulin,
- ACE2 inhibitors (for example, enalapril)
- angiotensin II receptor blockers (for example, losartan)
- and DPP4 inhibitors (for instance sitagliptin)
Although there is no substantial data to support the discontinuation of these drugs when you contract COVID-19 with diabetes, it is still a good idea to consult your physician to discuss any changes you might be experiencing [6].
Here is a step-by-step guide to recovering from COVID-19 and avoiding its complications if you have diabetes:
Managing Acute Complications
The first preventive measure is immediately detecting and treating acute complications, such as hyperglycemia and hypoglycemia.
If you have diabetes and you contract COVID-19, there is a need to start managing hyperglycemia (high blood sugar) aggressively. This is because, due to the infection, there will be significant hyperglycemia owing to the inflammation and stress of the disease itself.
While episodes of hyperglycemia are more common in COVID-19 patients, there is also a possibility of hypoglycemic (low blood sugar) events.

The use of hydroxychloroquine has been mainly linked with hypoglycemia in diabetics [6].
So, be watchful of these events, and act according to the advice and recommendations of your healthcare provider.

Laboratory Examinations
The second step is to have your recent blood sugar and ketone test results available in case your physician needs to see them.
If the results show moderate to large ketones, you should seek medical help immediately.
Depending on your condition, the doctor may advise having some lab tests done.
The results of these tests may show:
- A decrease in white blood cells
- Elevated neutrophil counts (if you have a severe case of COVID-19)
- Positive D-dimer
- An increase in blood urea and creatinine levels
According to your test results, your doctor will prescribe the necessary medicines to restore these parameters.
In some cases, getting hospitalized for proper management of diabetes and COVID-19 is suggested.
Managing Mental Health After COVID-19
It has been estimated that up to 87% of people affected with Type 2 diabetes are “emotionally distressed.”
Since stress and anxiety can trigger hyperglycemia in diabetic patients, it is crucial to make sure these disorders are adequately addressed.
Being physically active can significantly keep stress at bay. Seeing friends and talking to someone about how you feel are also good ways to manage stress, anxiety, and depression during the pandemic.

Why Is It Important to Seek Medical Help?
For most people, COVID-19 symptoms are not severe and can be easily managed at home.
However, things can differ for older people or those with underlying health conditions, including Type 1 and Type 2 diabetes.
As a person with diabetes, you must be aware that it’s possible to experience more severe symptoms when contracting the virus and may require medical attention.
It is particularly important to watch out for the following signs and seek medical help immediately if you experience any of these:
- Persistent chest pain
- Difficulty in breathing
- Disorientation
- Bluish lips
If you would like to further education or take the prediabetes survey, visit HCPSC National Diabetes Prevention & Management Program for more information.
Managing COVID-19 With Diabetes
While people with diabetes may face a higher risk of severe illness and complications from COVID-19, proper and timely management can save lives.
Here is a summary of various options available to you as a patient, which you must use in addition to following preventive measures like washing hands, social distancing, and wearing masks.
Diabetes self-management
The first and foremost step during this time is to self-manage your condition as much as possible. Since people are advised to stay home and keep a distance from others when infected with the virus, self-management can significantly improve their glycemic control and minimize their risk of developing complications.
The following is a list of self-management steps you can take, especially if you have limited access to COVID-related health services:
- Regular monitoring of your blood sugar
- Healthy eating
- Being physically active
- Use of prescribed medications on time
Telemedicine
Telemedicine has become an increasingly popular option for diabetes management during the pandemic. Health Care Partners of South Carolina allows patients to communicate with their healthcare providers remotely and receive guidance on self-care and medication management from the safety of their own homes.
Even if you haven’t contracted the virus yet, using this facility for virtual consultations is advisable.


Getting Vaccinated
In addition to focusing on healthy eating and regular exercise, healthcare experts emphasize the importance of staying current with recommended COVID-19 vaccinations and boosters to support the immune system of people with diabetes.
Other vaccines are also advised, such as the Flu vaccine and Pneumovax. Please speak with your healthcare provider at HCPSC when you have your next visit to inquire if you are due for these lifesaving vaccines.
COVID-19 vaccines work to stimulate the body’s natural defenses, creating immunity to the coronavirus and its variants. However, many people do not get an updated booster necessary for better protection against COVID-19. A third dose of vaccine is particularly recommended for immune-compromised people, including people with diabetes.
